Neuralgia Trigeminal: Uncover 9 risky causes of this debilitating condition and learn prevention tips for lasting relief. Understanding neuralgia trigeminal is key for effective management.

Table of Contents
Recognizing the signs of neuralgia trigeminal is essential for timely diagnosis and treatment.
Neuralgia Trigeminal: 9 Risky Causes to Watch
Neuralgia trigeminal can cause significant distress and understanding its causes can lead to better management strategies.
Imagine a pain so intense, it’s been dubbed “the suicide disease.” 😱 This isn’t your average headache or toothache – it’s trigeminal neuralgia, a condition that can turn even the simplest actions like brushing your teeth or sipping a cup of coffee into excruciating ordeals. But what causes this debilitating condition? Here, we delve into the various aspects of neuralgia trigeminal.
The truth about neuralgia trigeminal is that it can be complex and multifactorial.
Awareness of neuralgia trigeminal triggers is vital for effective symptom management.
Understanding neuralgia trigeminal is essential for anyone suffering from or at risk of this condition. The triggers and causes are complex, with many patients experiencing varying symptoms linked to neuralgia trigeminal.
In this blog post, we’ll dive deep into the 9 risky causes of neuralgia trigeminal that you need to watch out for. From genetic predispositions to surprising environmental triggers, we’ll explore the full spectrum of factors that could be behind your facial pain. So, buckle up as we embark on this journey to unravel the mysteries of neuralgia trigeminal and arm you with the knowledge to better manage and prevent this challenging condition. 🧠💪
While some triggers of trigeminal neuralgia are well-known, there are several risky causes that often fly under the radar. These hidden culprits could be silently wreaking havoc on your nervous system, leading to sudden, shocking bouts of facial pain. Understanding these less common but potentially dangerous factors is crucial for anyone dealing with or at risk of developing this condition.
In this blog post, we’ll dive deep into the 9 risky causes of trigeminal neuralgia that you need to watch out for. From genetic predispositions to surprising environmental triggers, we’ll explore the full spectrum of factors that could be behind your facial pain. So, buckle up as we embark on this journey to unravel the mysteries of trigeminal neuralgia and arm you with the knowledge to better manage and prevent this challenging condition. 🧠💪
Understanding Trigeminal Neuralgia
Neuralgia Trigeminal: Understanding Its Impact
Definition and symptoms
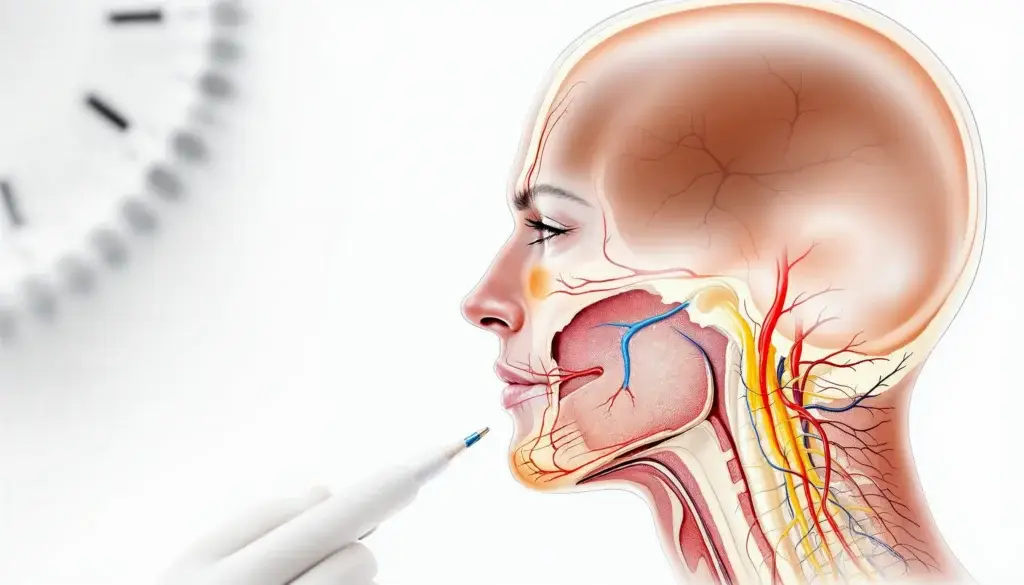
Trigeminal neuralgia (TN) is a chronic pain condition that affects the trigeminal nerve, one of the largest nerves in the head. This debilitating disorder is characterized by intense, episodic facial pain that can be triggered by even the slightest touch or movement. Patients often describe the pain as electric shock-like, stabbing, or burning sensations that can last from a few seconds to several minutes.
The primary symptoms of trigeminal neuralgia include:
- Sudden, severe facial pain
- Pain triggered by routine activities (e.g., eating, talking, brushing teeth)
- Episodes of pain lasting from a few seconds to several minutes
- Periods of remission between pain attacks
- Pain typically affecting one side of the face
It’s important to note that trigeminal neuralgia can be classified into two main types:
| Type | Description | Characteristics |
|---|---|---|
| Type 1 (TN1) | Classic TN | Sharp, shooting pain; periods of remission |
| Type 2 (TN2) | Atypical TN | Constant aching, burning pain; less common |
Areas affected by the condition
The trigeminal nerve has three main branches, each responsible for different areas of the face:
- Ophthalmic nerve (V1): Forehead, upper eyelid, and eye
- Maxillary nerve (V2): Lower eyelid, cheek, nostril, upper lip, and upper gum
- Mandibular nerve (V3): Jaw, lower lip, lower gum, and some muscles used for chewing
Trigeminal neuralgia can affect one or more of these branches, with the maxillary and mandibular branches being the most commonly affected. The pain is usually limited to one side of the face, although in rare cases, it can occur bilaterally.
Impact on quality of life
Neuralgia trigeminal often manifests in troubling ways, impacting daily lives significantly. Understanding which areas of the face are affected by neuralgia trigeminal is vital for proper diagnosis and management.
Trigeminal neuralgia can have a profound impact on a person’s quality of life, affecting various aspects of daily functioning and emotional well-being:
- Physical limitations: Many patients avoid activities that may trigger pain, leading to decreased physical activity and social isolation.
- Emotional distress: The unpredictable nature of pain attacks can cause anxiety, depression, and fear of future episodes.
- Sleep disturbances: Pain attacks or fear of attacks during sleep can lead to insomnia and fatigue.
- Dietary changes: Difficulty eating or drinking due to pain can result in weight loss and nutritional deficiencies.
- Social and occupational impairment: The condition may interfere with work, social relationships, and overall daily functioning.
Given the severe impact of trigeminal neuralgia on patients’ lives, early diagnosis and appropriate treatment are crucial. As we explore the common causes of this condition in the next section, it’s important to remember that understanding the underlying mechanisms can lead to more effective management strategies and improved quality of life for those affected by this challenging disorder.
Common Causes of Trigeminal Neuralgia
Trigeminal neuralgia, or neuralgia trigeminal, can affect one or more branches of the trigeminal nerve, leading to episodes of excruciating pain that warrant immediate attention.
A. Compression of the trigeminal nerve
Given the severe impact of neuralgia trigeminal on patients’ lives, understanding potential causes is crucial for effective management.
Compression of the trigeminal nerve is the most common cause of trigeminal neuralgia (TN). This typically occurs when a blood vessel, usually an artery, presses against the nerve at its root near the brainstem. Over time, this constant pressure can wear away the protective myelin sheath surrounding the nerve, leading to hypersensitivity and the characteristic pain associated with TN.
There are several ways in which compression can occur:
- Vascular compression: Blood vessels pressing on the nerve
- Tumor growth: Benign or malignant growths near the nerve
- Bone abnormalities: Skull base deformities or bony spurs
- Aneurysms: Enlarged blood vessels causing pressure
| Compression Type | Description | Prevalence |
|---|---|---|
| Vascular | Blood vessel pressure | Most common |
| Tumor | Growth near nerve | Less common |
| Bone | Skull base deformities | Rare |
| Aneurysm | Enlarged blood vessels | Very rare |
B. Multiple sclerosis
Multiple sclerosis (MS) is a significant risk factor for developing trigeminal neuralgia. In fact, TN is often one of the first symptoms that leads to an MS diagnosis. The connection between MS and TN lies in the demyelination process characteristic of MS, which affects the nervous system, including the trigeminal nerve.
Key points about MS and TN:
Neuralgia trigeminal can significantly impact daily life, emphasizing the need for awareness.
Identifying which of the risky causes may lead to neuralgia trigeminal is essential for prevention and treatment strategies.
Understanding neuralgia trigeminal is essential for finding effective treatments.
- Approximately 2-4% of MS patients develop TN
- TN symptoms in MS patients are often bilateral (affecting both sides)
- MS-related TN may be more challenging to treat than other forms
C. Tumors affecting the trigeminal nerve
While less common than vascular compression, tumors can also cause trigeminal neuralgia by exerting pressure on the nerve. These tumors can be benign or malignant and may originate from various tissues near the trigeminal nerve.
Types of tumors associated with TN include:
- Acoustic neuromas
- Meningiomas
- Epidermoid cysts
- Schwannomas
It’s important to note that tumors causing TN are typically slow-growing and may not present other symptoms initially, making early detection crucial.
D. Aging and nerve deterioration
As we age, our nerves naturally undergo changes that can increase susceptibility to conditions like trigeminal neuralgia. The aging process can lead to:
- Thinning of the myelin sheath
- Reduced nerve elasticity
- Increased vulnerability to compression
- Slower nerve regeneration
These age-related changes can make the trigeminal nerve more sensitive to stimuli and prone to developing TN. Additionally, the cumulative effects of other risk factors over time may contribute to the onset of TN in older individuals.
Understanding these common causes of trigeminal neuralgia is crucial for proper diagnosis and treatment. While compression of the trigeminal nerve remains the primary cause, it’s essential to consider other factors such as multiple sclerosis, tumors, and age-related changes. By identifying the underlying cause, healthcare professionals can develop more targeted and effective treatment strategies for individuals suffering from this painful condition.
Less Common but Risky Causes
Blood vessel abnormalities
Blood vessel abnormalities can be a less common but potentially risky cause of trigeminal neuralgia. These abnormalities may lead to compression or irritation of the trigeminal nerve, resulting in severe facial pain. Some of the most notable blood vessel issues include:
- Arteriovenous malformations (AVMs)
- Aneurysms
- Vascular loops
Let’s explore these abnormalities in more detail:
Arteriovenous malformations (AVMs)
Awareness of neuralgia trigeminal symptoms can lead to quicker interventions.
AVMs are tangles of abnormal blood vessels that can form in various parts of the body, including the brain. When an AVM develops near the trigeminal nerve, it can cause compression and lead to trigeminal neuralgia. These malformations are typically congenital but may not cause symptoms until later in life.
Aneurysms
An aneurysm is a bulge or ballooning in a blood vessel wall. When an aneurysm forms near the trigeminal nerve, it can put pressure on the nerve, triggering pain. Although rare, aneurysms in this area can be particularly dangerous if they rupture, potentially leading to life-threatening complications.
Vascular loops
Vascular loops occur when blood vessels take an unusual path, sometimes wrapping around or pressing against the trigeminal nerve. This compression can cause the nerve to malfunction, resulting in trigeminal neuralgia symptoms.
| Blood Vessel Abnormality | Description | Potential Risk |
|---|---|---|
| AVMs | Tangles of abnormal blood vessels | Compression of trigeminal nerve |
| Aneurysms | Bulge in blood vessel wall | Pressure on nerve, risk of rupture |
| Vascular loops | Unusual blood vessel path | Compression and nerve malfunction |
Facial trauma or injury
Facial trauma or injury can be another less common but significant cause of trigeminal neuralgia. Various types of facial injuries can potentially damage or compress the trigeminal nerve, leading to chronic pain. Some examples include:
Neuralgia trigeminal is often misunderstood, which can delay proper care.
- Blunt force trauma from accidents or falls
- Facial fractures
- Penetrating injuries
In some cases, even minor facial injuries can trigger trigeminal neuralgia if they affect the nerve’s function or surrounding structures.
Dental procedures gone wrong
While dental procedures are generally safe, complications can occasionally occur that may lead to trigeminal neuralgia. Some potential issues include:
- Nerve damage during tooth extraction
- Improper placement of dental implants
- Complications from root canal treatments
These situations can result in direct injury to the trigeminal nerve or create inflammation that puts pressure on the nerve, causing pain.
Viral infections
Certain viral infections can potentially trigger trigeminal neuralgia or exacerbate existing conditions. Some viruses known to affect the trigeminal nerve include:
- Herpes simplex virus (HSV)
- Varicella-zoster virus (VZV)
- Epstein-Barr virus (EBV)
These infections can cause inflammation or damage to the nerve, leading to pain and other symptoms associated with trigeminal neuralgia.
Understanding these less common but risky causes of trigeminal neuralgia is crucial for proper diagnosis and treatment. If you experience persistent facial pain, it’s essential to consult with a healthcare professional to determine the underlying cause and develop an appropriate treatment plan. In the next section, we’ll explore the genetic and hereditary factors that may contribute to the development of trigeminal neuralgia.
Genetic and Hereditary Factors
Family history of trigeminal neuralgia
While trigeminal neuralgia is not typically considered a hereditary condition, recent studies have shown that there may be a genetic component to its development. Individuals with a family history of trigeminal neuralgia are at a slightly higher risk of developing the condition themselves. This familial link suggests that certain genetic factors may predispose some people to trigeminal neuralgia.
Research has shown that approximately 4-6% of patients with trigeminal neuralgia have a first-degree relative (parent, sibling, or child) who also suffers from the condition. This prevalence is higher than what would be expected by chance alone, indicating a potential genetic influence.
Genetic mutations linked to the condition
Several genetic mutations have been identified as potentially contributing to the development of trigeminal neuralgia. These mutations primarily affect genes involved in nerve function and pain signaling pathways. Some of the key genetic factors associated with trigeminal neuralgia include:
- Sodium channel gene mutations
- Potassium channel gene variants
- Calcium channel gene alterations
- Genes involved in myelin production and maintenance
The following table summarizes some of the most significant genetic mutations linked to trigeminal neuralgia:
| Gene | Function | Associated Mutation |
|---|---|---|
| SCN9A | Sodium channel | Gain-of-function mutations |
| KCNS1 | Potassium channel | Single nucleotide polymorphisms |
| CACNA1A | Calcium channel | Missense mutations |
| MBP | Myelin basic protein | Altered expression levels |
Inherited disorders affecting nerve function
Several inherited disorders can increase the risk of developing trigeminal neuralgia or similar neuropathic facial pain conditions. These disorders often affect the structure or function of nerves, making individuals more susceptible to trigeminal nerve compression or irritation. Some of the inherited disorders associated with an increased risk of trigeminal neuralgia include:
- Multiple sclerosis (MS): Although not strictly hereditary, there is a genetic component to MS susceptibility. MS can cause demyelination of nerves, including the trigeminal nerve, potentially leading to trigeminal neuralgia.
- Charcot-Marie-Tooth disease: This inherited neurological disorder affects peripheral nerves and can sometimes involve cranial nerves, including the trigeminal nerve.
- Hereditary neuropathies: Various inherited neuropathies can affect the trigeminal nerve, increasing the risk of developing trigeminal neuralgia.
- Ehlers-Danlos syndrome: This group of inherited connective tissue disorders can sometimes affect nerve function and increase susceptibility to nerve compression.
It’s important to note that while these genetic and hereditary factors may increase the risk of developing trigeminal neuralgia, they do not guarantee its occurrence. Environmental factors, lifestyle choices, and other medical conditions also play significant roles in the development of this painful condition.
Understanding the genetic and hereditary factors associated with trigeminal neuralgia can help in early identification of at-risk individuals and potentially lead to more targeted prevention and treatment strategies. As research in this area continues to advance, we may gain further insights into the complex interplay between genetics and trigeminal neuralgia, paving the way for more personalized approaches to managing this challenging condition.
Lifestyle and Environmental Triggers
Stress and anxiety
Stress and anxiety are significant lifestyle factors that can trigger or exacerbate trigeminal neuralgia (TN) symptoms. The relationship between these psychological factors and TN is complex, but understanding it can help manage the condition more effectively.
- Stress-induced muscle tension: Heightened stress levels can cause facial muscles to tense up, potentially compressing the trigeminal nerve.
- Hormonal changes: Stress triggers the release of cortisol and other hormones, which may increase nerve sensitivity.
- Lowered pain threshold: Anxiety can make individuals more susceptible to perceiving pain, amplifying TN symptoms.
To manage stress-related TN triggers, consider:
- Mindfulness meditation
- Regular exercise
- Cognitive-behavioral therapy
- Adequate sleep
Extreme temperatures
Temperature fluctuations can be a significant trigger for trigeminal neuralgia attacks. Both hot and cold extremes can affect nerve function and sensitivity.
| Temperature | Effect on TN |
|---|---|
| Cold | Can cause blood vessels to constrict, potentially irritating the trigeminal nerve |
| Hot | May lead to increased nerve activity and sensitivity |
To minimize temperature-related triggers:
- Use a scarf or face mask in cold weather
- Avoid sudden temperature changes
- Use lukewarm water for face washing and oral hygiene
Certain foods and beverages
Diet can play a crucial role in managing trigeminal neuralgia. Some individuals find that certain foods and drinks can trigger or worsen their symptoms.
Common dietary triggers include:
- Caffeinated beverages
- Alcohol
- Spicy foods
- Citrus fruits
- Artificially sweetened products
It’s essential to keep a food diary to identify personal triggers. Eliminating or reducing consumption of problematic items can help manage TN symptoms effectively.
Physical exertion
Physical activities, especially those involving facial movements or vibrations, can potentially trigger trigeminal neuralgia attacks. This includes:
- Vigorous exercise
- Talking or laughing excessively
- Chewing tough foods
- Brushing teeth
To minimize the risk of triggering TN symptoms during physical activities:
- Start with low-impact exercises and gradually increase intensity
- Practice proper form and technique to reduce unnecessary facial tension
- Take frequent breaks during activities that involve repetitive facial movements
- Use adaptive tools for daily tasks (e.g., electric toothbrushes with soft bristles)
Understanding these lifestyle and environmental triggers is crucial for effectively managing trigeminal neuralgia. By identifying personal triggers and making appropriate adjustments, individuals can significantly reduce the frequency and severity of TN attacks. However, it’s important to note that trigger management should be part of a comprehensive treatment plan developed in consultation with a healthcare professional.
With this understanding of lifestyle and environmental factors, we can now explore the various medical conditions associated with trigeminal neuralgia, which can provide further insight into the complexity of this painful disorder.
Medical Conditions Associated with Trigeminal Neuralgia
Hypertension
Hypertension, or high blood pressure, has been linked to an increased risk of developing trigeminal neuralgia (TN). The relationship between hypertension and TN is complex, but research suggests that elevated blood pressure can contribute to the compression or irritation of the trigeminal nerve. This compression is often the root cause of the intense facial pain associated with TN.
| Hypertension and TN | Impact |
|---|---|
| Blood vessel changes | Thickening and hardening of arteries |
| Nerve compression | Increased pressure on trigeminal nerve |
| Pain frequency | May increase episodes of facial pain |
| Treatment complications | Can affect medication effectiveness |
Patients with hypertension should be particularly vigilant about monitoring their blood pressure and adhering to their prescribed treatment regimen. Proper management of hypertension may help reduce the risk of developing TN or alleviate symptoms in those already affected.
Diabetes
Diabetes is another medical condition that has been associated with an increased risk of trigeminal neuralgia. The connection between diabetes and TN is primarily due to the neuropathic effects of prolonged high blood sugar levels on the nervous system.
Key points to consider:
- Diabetic neuropathy can affect cranial nerves, including the trigeminal nerve
- Elevated blood sugar levels may damage the myelin sheath protecting nerve fibers
- Microvascular changes in diabetes can impact blood supply to nerves
- Diabetes-related inflammation may contribute to nerve irritation and pain
Individuals with diabetes should work closely with their healthcare providers to maintain optimal blood sugar control. This approach may help reduce the risk of developing TN or minimize its severity if already present.
Autoimmune disorders
Various autoimmune disorders have been linked to an increased incidence of trigeminal neuralgia. These conditions, where the immune system mistakenly attacks healthy tissues, can potentially affect the trigeminal nerve or its surrounding structures.
Some autoimmune disorders associated with TN include:
- Multiple Sclerosis (MS)
- Lupus
- Sjögren’s syndrome
- Rheumatoid Arthritis
In the case of multiple sclerosis, demyelination of nerve fibers can directly impact the trigeminal nerve, leading to TN symptoms. For other autoimmune conditions, the relationship may be due to inflammation or vascular changes that affect the nerve.
| Autoimmune Disorder | Potential TN Mechanism |
|---|---|
| Multiple Sclerosis | Demyelination of trigeminal nerve |
| Lupus | Vascular inflammation and damage |
| Sjögren’s syndrome | Nerve compression from inflamed salivary glands |
| Rheumatoid Arthritis | Systemic inflammation affecting nerves |
Patients with autoimmune disorders should be aware of the potential for developing TN and report any facial pain symptoms to their healthcare provider promptly. Managing the underlying autoimmune condition effectively may help reduce the risk or severity of TN.
Now that we’ve explored the medical conditions associated with trigeminal neuralgia, it’s crucial to understand how healthcare professionals diagnose and assess this painful condition. Let’s move on to the next section, which covers the diagnostic process and medical evaluation for trigeminal neuralgia.
Diagnosis and Medical Assessment
Prevention and management strategies for neuralgia trigeminal are crucial for improving overall quality of life and reducing the frequency of painful episodes.
Physical examination techniques
When diagnosing trigeminal neuralgia, healthcare professionals employ various physical examination techniques to assess the patient’s symptoms and identify potential triggers. These techniques are crucial in determining the nature and severity of the condition.
- Facial sensation testing: The doctor will use light touch, pinpricks, or temperature stimuli to evaluate the sensitivity of different areas of the face.
- Trigger point identification: Gentle pressure is applied to specific facial areas to locate points that trigger pain.
- Jaw movement assessment: The physician will observe and evaluate jaw movements to check for any abnormalities or pain triggers.
- Corneal reflex test: This involves lightly touching the cornea to assess the trigeminal nerve’s function.
Imaging tests for accurate diagnosis
Imaging tests play a vital role in accurately diagnosing trigeminal neuralgia and identifying any underlying causes. These tests help visualize the trigeminal nerve and surrounding structures, allowing healthcare providers to detect abnormalities or compression.
| Imaging Test | Purpose | Advantages |
|---|---|---|
| MRI (Magnetic Resonance Imaging) | Detailed images of brain and nerve structures | Non-invasive, high-resolution images |
| MRA (Magnetic Resonance Angiography) | Visualizes blood vessels | Detects vascular compression |
| CT (Computed Tomography) scan | Bone and soft tissue imaging | Quick, useful for detecting tumors |
In some cases, specialized imaging techniques such as high-resolution MRI or diffusion tensor imaging may be employed for a more detailed examination of the trigeminal nerve and its branches.
Awareness of neuralgia trigeminal can empower patients in managing their care.
Ruling out other conditions
Trigeminal neuralgia can sometimes be confused with other conditions that cause facial pain. Therefore, it’s essential to rule out these conditions during the diagnostic process. Some of the conditions that may mimic trigeminal neuralgia include:
- Dental problems (e.g., tooth abscess, temporomandibular joint disorders)
- Sinusitis
- Cluster headaches
- Postherpetic neuralgia
- Multiple sclerosis
To differentiate trigeminal neuralgia from these conditions, healthcare providers may:
- Review the patient’s medical history thoroughly
- Conduct additional tests, such as blood work or nerve conduction studies
- Consult with specialists in neurology, dentistry, or otolaryngology
By employing a combination of physical examination techniques, advanced imaging tests, and careful consideration of other potential causes, healthcare professionals can accurately diagnose trigeminal neuralgia. This comprehensive approach ensures that patients receive the most appropriate treatment for their specific condition.
As we move forward, we’ll explore the various treatment options available for trigeminal neuralgia, including their potential risks and benefits. Understanding these options is crucial for developing an effective management strategy tailored to each patient’s needs.
Treatment Options and Their Risks
Medications and potential side effects
When it comes to treating trigeminal neuralgia, medications are often the first line of defense. However, it’s crucial to understand both their benefits and potential risks. Here’s a breakdown of common medications and their side effects:
| Medication Type | Examples | Common Side Effects |
|---|---|---|
| Anticonvulsants | Carbamazepine, Gabapentin | Dizziness, drowsiness, nausea |
| Antispasmodics | Baclofen | Weakness, confusion, insomnia |
| Antidepressants | Amitriptyline, Nortriptyline | Dry mouth, weight gain, constipation |
| Opioids | Oxycodone, Tramadol | Addiction risk, constipation, nausea |
It’s important to note that while these medications can provide significant relief, they may lose effectiveness over time, requiring dosage adjustments or medication changes.
Surgical interventions and complications
For patients who don’t respond well to medications or experience intolerable side effects, surgical options may be considered. These procedures aim to reduce pressure on the trigeminal nerve or interrupt pain signals:
- Microvascular decompression (MVD)
- Gamma Knife radiosurgery
- Percutaneous rhizotomy techniques
While often effective, these surgeries come with potential risks:
- Facial numbness or weakness
- Hearing loss
- Cerebrospinal fluid leaks
- Stroke (rare)
- Infection
The choice of surgical intervention depends on the patient’s age, overall health, and the specific nature of their trigeminal neuralgia.
Alternative therapies and their efficacy
For those seeking non-invasive options or complementary treatments, several alternative therapies have shown promise in managing trigeminal neuralgia:
- Acupuncture: May help reduce pain intensity and frequency
- Biofeedback: Teaches patients to control certain bodily processes
- Vitamin B12 supplements: May support nerve health
- Botox injections: Can provide temporary relief for some patients
While these therapies can be beneficial, their efficacy varies among individuals. It’s crucial to discuss these options with a healthcare provider before incorporating them into a treatment plan.
Now that we’ve explored the various treatment options and their associated risks, it’s essential to consider how to prevent flare-ups and manage this condition long-term. Let’s move on to discuss prevention and management strategies that can help individuals with trigeminal neuralgia maintain a better quality of life.
Prevention and Management Strategies
Identifying and avoiding triggers
Identifying and avoiding triggers is crucial for managing trigeminal neuralgia (TN) effectively. Common triggers include:
- Temperature changes
- Facial movements
- Certain foods and drinks
- Loud noises
- Stress
To help identify your specific triggers, consider keeping a pain diary. Record the following information:
| Date | Time | Pain Level (1-10) | Activity | Food/Drink | Weather | Notes |
|---|---|---|---|---|---|---|
By analyzing this data, you can pinpoint patterns and avoid potential triggers. Some general tips for trigger avoidance include:
- Use a straw for cold drinks
- Wear a scarf or face mask in cold weather
- Practice gentle oral hygiene
- Avoid hard or crunchy foods
Stress reduction techniques
Stress is a common trigger for TN flare-ups. Implementing stress reduction techniques can significantly improve symptom management:
- Mindfulness meditation
- Deep breathing exercises
- Progressive muscle relaxation
- Yoga or gentle stretching
- Guided imagery
Consistency is key when practicing these techniques. Aim for at least 10-15 minutes daily to experience the full benefits.
Consulting with professionals about neuralgia trigeminal is essential for successful management.
Regular medical check-ups
Maintaining regular appointments with your healthcare provider is essential for managing trigeminal neuralgia. These check-ups allow for:
Being proactive about neuralgia trigeminal can improve outcomes significantly.
- Monitoring of symptom progression
- Adjustment of medication dosages
- Early detection of potential complications
- Discussion of new treatment options
Prepare for your appointments by keeping a list of questions and concerns. This ensures you make the most of your time with your healthcare provider.
Lifestyle modifications for symptom control
Making certain lifestyle changes can help control TN symptoms and improve overall quality of life:
- Diet modifications:
- Avoid trigger foods (e.g., spicy, acidic, or extremely hot/cold items)
- Incorporate anti-inflammatory foods (e.g., fatty fish, berries, leafy greens)
- Sleep hygiene:
- Maintain a consistent sleep schedule
- Create a relaxing bedtime routine
- Ensure a comfortable sleep environment
- Physical activity:
- Engage in low-impact exercises (e.g., swimming, walking)
- Practice gentle facial exercises as recommended by your healthcare provider
- Alternative therapies:
- Acupuncture
- Biofeedback
- Herbal supplements (consult with your doctor first)
By implementing these prevention and management strategies, individuals with trigeminal neuralgia can better control their symptoms and improve their overall quality of life. Remember that TN management is often a process of trial and error, so patience and persistence are key. With the right combination of medical treatment and lifestyle modifications, many people with TN can achieve significant symptom relief and lead fulfilling lives.
Trigeminal neuralgia is a complex and often debilitating condition with various potential causes. From common triggers like vascular compression to less frequent but serious factors such as tumors or multiple sclerosis, understanding the root of this condition is crucial for effective management. Genetic predisposition, lifestyle choices, and certain medical conditions can all play a role in the development or exacerbation of trigeminal neuralgia.
Recognizing the signs and seeking prompt medical assessment is key to proper diagnosis and treatment. While various treatment options exist, each comes with its own set of risks and benefits. By staying informed about potential triggers and implementing appropriate prevention strategies, individuals can take proactive steps to manage their condition and improve their quality of life. If you suspect you may be experiencing symptoms of trigeminal neuralgia, consult with a healthcare professional to explore the best course of action for your specific situation.
“10 Proven Health Benefits of Probiotics You Need to Know”
As we explore the medical conditions associated with neuralgia trigeminal, understanding their mechanisms can enhance management strategies.
Diagnosis of neuralgia trigeminal is often multifaceted, involving various physical examination techniques that aid in identifying the condition.
Advanced imaging tests are particularly useful for visualizing potential compression of the trigeminal nerve, essential for diagnosing neuralgia trigeminal.
By recognizing the signs and seeking prompt medical assessment, individuals experiencing symptoms of neuralgia trigeminal can access tailored treatment options.
Managing neuralgia trigeminal effectively requires understanding its triggers.
Effective management of neuralgia trigeminal requires a multi-faceted approach.
Understanding neuralgia trigeminal symptoms aids in seeking timely treatment.
Identifying symptoms of neuralgia trigeminal can lead to better outcomes.

Share this content:
